brandkit
Brand Kit Brand Kit Brand Colors #CC2C7C #DC4C5C #020202 #989898 #FFFFFF Logos & Icons Small Logo Download Copy Link Brand Icon Download Copy Link
Are your loved one’s memories slowly fading away? Do they struggle with recalling your name? This is a painful reality for many families and caregivers dealing with vascular dementia in their elderly loved ones.
In this article, we will explore the progression of vascular dementia stages and offer insights into how to navigate this challenging journey with your loved ones.
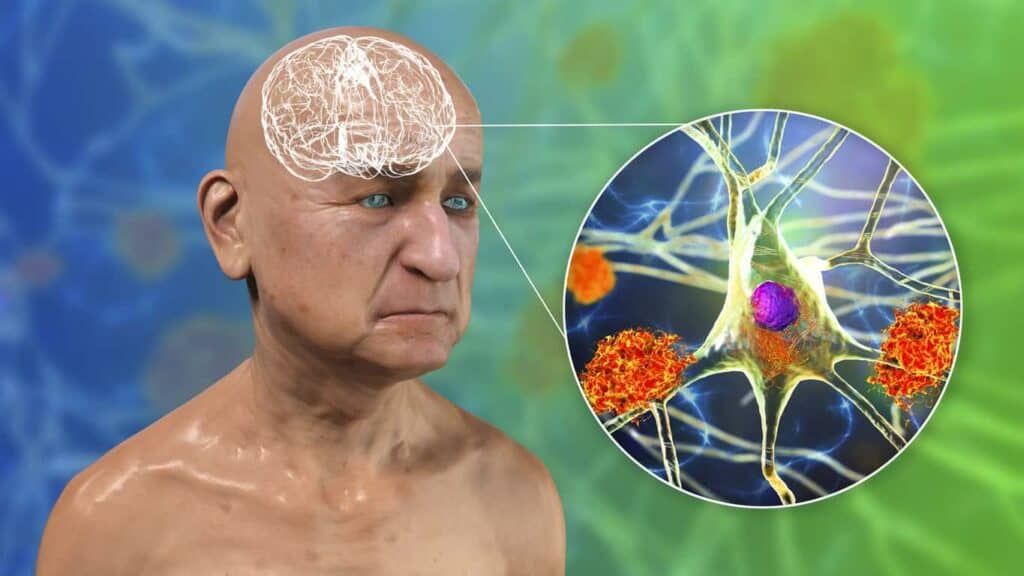
Vascular dementia is a type of dementia that is characterized by a decline in cognitive function due to impaired blood flow to the brain. It is the second most common cause of dementia after Alzheimer’s disease.
There are different types of vascular dementia classified on the basis of causes and symptoms. They include:
Vascular dementia is caused by problems in blood circulation within the central nervous system that damage brain tissue and cause a subsequent decline in a person’s cognitive abilities. These can include disorders like stroke, atherosclerosis (narrowing and hardening of the arteries), high blood pressure, diabetes, and other vascular diseases.
The severity and progression of vascular dementia can differ from person to person, based on the extent of damage and the affected areas of the brain. Older people, especially those who have experienced one or more strokes in the past are at a particularly high risk.

Memory loss and cognitive decline are hallmark symptoms of vascular dementia. The elderly may find difficulty in recalling recent events or retaining new information. In daily routine, they may not remember the names of close loved ones, forget about their appointments, repeat questions, and appear agitated in familiar gatherings.
Vascular dementia can lead to significant alterations in mood and personality. Seniors may experience emotional disturbances, including irritability, depression, or apathy. You might observe increased impulsiveness and social withdrawal in them.
As cognitive abilities decline, older people with vascular dementia often have difficulty with activities of daily living (ADLs). This can include managing finances, prepping meals, and maintaining personal hygiene. They may not even remember how to use basic household appliances, which can frustrate them and lead to a loss of independence.
Vascular dementia also results in physical symptoms, such as weakness, tremors, loss of speech, difficulty walking, and issues with coordination. These physical challenges impact their level of independence and quality of life, making mobility and self-care more difficult.
Early diagnosis is important in managing vascular dementia as it helps treat the underlying causes, manage risk factors, and plan strategies to slow down the progression.
The treatment of vascular dementia may include:
Support from families, caregivers, and healthcare teams is essential in providing the elderly with the necessary care and assistance.
Vascular dementia has a significant impact on older people owing to its relation with age-related conditions like stroke and atherosclerosis. The prevalence of vascular dementia is expected to increase with an increase in the number of the aging population. This not only affects the elderly with vascular dementia but also puts more emotional and financial burden on their families and healthcare systems.
The cognitive and functional changes in vascular dementia typically progress through many stages. Not every senior with vascular dementia will experience the exact same symptoms, and everyone might not experience all these stages.
The progression may also be influenced by factors such as overall health, treatment, and lifestyle. However, here is an overview of the seven common stages of vascular dementia:
In the initial stage, seniors with vascular dementia may not exhibit any visible symptoms or changes in cognitive function. It is also characterized by good overall cognitive function, with no significant memory loss or other cognitive impairments.
In this stage, the elderly may begin to experience some kind of subtle cognitive changes. They may have trouble remembering, concentrating, and solving problems, which can be mistaken for normal forgetfulness as they age. Functional abilities are generally preserved, and they can still perform everyday tasks independently.
Cognitive deficits become more evident during this stage. Seniors may struggle with memory and exhibit difficulties in planning, organizing, and decision-making. Some mild personality and mood changes may become noticeable, such as irritability or frustration. Although independence in daily activities is still maintained, assistance and support become increasingly necessary.
As vascular dementia progresses, the cognitive impairments become more severe. Memory loss becomes pronounced, making it challenging for the elderly to remember recent events or even familiar faces.
Communication difficulties may emerge, with older people having trouble finding the right words or following a conversation. Everyday activities, such as dressing and bathing, may require significant assistance and supervision.
In this stage, seniors may struggle to recognize loved ones and become increasingly disoriented about time and place. Cognitive and functional abilities continue to deteriorate, making it difficult to perform most activities of daily living without constant assistance.
Severe cognitive impairment characterizes this stage. Older people in this stage may have little to no ability to communicate or understand spoken language. They may be unable to control their bodily functions, such as bladder or bowel movements. Mobility may also be significantly impaired, necessitating full-time care and support.
In the final stage, seniors lose almost all cognitive and functional abilities. They are typically bedridden, unable to speak, and require 24/7 care for all aspects of daily life, including feeding and hygiene. The elderly in this stage are highly vulnerable to other health issues, and they have reduced life expectancy.

Vascular dementia not only impacts the affected elderly but also has a lasting effect on their family, loved ones, and caregivers. Let’s discuss the support options available for the elderly with vascular dementia that can make this journey easier for both patients and their caregivers.
Family plays a crucial role in providing care and support that can significantly impact the patient’s quality of life. For the elderly with vascular dementia, having familiar faces around, who understand their history and preferences, can be comforting. Moreover, family involvement creates a consistent and secure environment that can help reduce anxiety and agitation, common symptoms of the condition.
It’s crucial for caregivers to recognize that they, too, need support. Engage in support groups or therapy to seek a safe space and share your experiences and emotions. It helps caregivers cope with the emotional toll of witnessing the gradual decline in their loved one’s cognitive abilities. Organizations like Alzheimer’s Association, offer resources, education, and connections to other caregivers facing similar challenges.
Rather than waiting for the disease to advance to a point where immediate care is necessary, transitioning to assisted living at an earlier stage can offer several advantages. It provides dementia patients and their families with the time to adapt to the new environment gradually.
Assisted living plays a crucial role in offering specialized care for elderly people during various stages of vascular dementia. These facilities are designed to cater to the specific needs of dementia patients in several ways.
The staff in assisted living facilities are trained to understand the unique challenges that the elderly with dementia face. They have the expertise and experience required to provide appropriate care. They are available around the clock to ensure that the older residents receive the care they need.
Another critical aspect of assisted living is safety. Vascular dementia often leads to cognitive decline, which can result in an increased risk of accidents and wandering. Assisted living areas are designed with safety in mind, including features like secured entry and exit points, alarm systems, and a secure environment that minimizes potential hazards.
Dementia often leads to isolation and a sense of loneliness but assisted living facilities actively promote social interaction. They organize various group activities, including art classes, group therapy, games, and communal dining, all of which foster social connections among residents. This helps combat the negative effects of isolation and enhances the overall quality of life for dementia patients.

In order to provide the best possible support for the elderly, you need to understand the progression of vascular dementia stages. By recognizing the signs, learning about the different stages, and exploring care options like assisted living, you can enhance the quality of life for your loved one.
Remember, you’re not alone in this journey. Together, we can face the challenges of vascular dementia with compassion, resilience, and a commitment to preserving the dignity and well-being of your elderly family members.
Contact us today to seek specialized assisted living for your loved ones with vascular dementia.
Get care >
Brand Kit Brand Kit Brand Colors #CC2C7C #DC4C5C #020202 #989898 #FFFFFF Logos & Icons Small Logo Download Copy Link Brand Icon Download Copy Link

Are you worried your loved one isn’t sleeping well? Do you notice them tossing and turning, napping in the afternoon, or complaining about fatigue most

There’s something deeply comforting about aging in a place that feels like home—the familiar walls, the cherished memories, the sense of belonging. For many older

Caring for an elderly loved one is a journey filled with love, challenges, and a lot of questions. One of the biggest questions you might

Amy's Eden Senior Care © 2023